Abstract
Introduction:Cellulitis of the soft tissue surrounding the face, jaw, and upper neck is referred to as maxillofacial cellulitis. Cellulitis is a purulent inflammation with a generally widespread scope that can affect all areas of the body. The most prevalent harmful bacteria are Staphylococcus aureus and Streptococcus, followed by Pneumococcus and Escherichia coli, which frequently cause mixed bacterial infections. If the target is eliminated and the infection is promptly under control, the prognosis is typically favorable. The reports of hematological conditions aggravated by maxillofacial fungal cellulitis are uncommon, and there are few accounts of clinical symptoms and results.
Method: Retrospective analysis was done on three patients with hematological diseases complicated by maxillofacial fungal cellulitis who were diagnosed and treated in our hospital between July 2014 and July 2022. The general information, clinical manifestations, diagnostic techniques, therapeutic drugs, and prognosis were all examined. Utilizing the terms "maxillofacialregion," "fungal cellulitis," "hematopathy," "maxillofacial," and "fungal cellulitis" in the CNKI, PubMed, Wanfang, and VIP databases, researchers were able to gather and assess pertinent domestic and international literature.
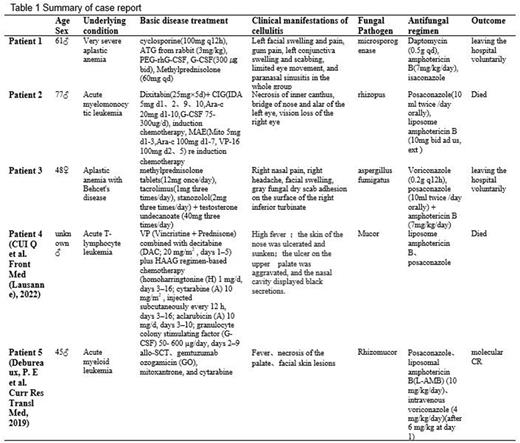
Result: Three patients from our institution and two patients who underwent a literature study had their clinical data compiled(Cui Q et al. Front Med (Lausanne), 2022; Debureaux, P. E et al. Curr Res Transl Med, 2019). The diagnosis of maxillofacial fungal cellulitis was determined based on the clinical signs, imaging features, and secretory pathogen culture, and mNGS was also carried out in three cases. Rhizopus Microspora, Aspergillus fumigatus, Mucor, and 2 instances of Rhizopus, of which 2 cases had mixed infections, were the pathogenic microorganisms. According to the kind and severity of the initial disease, two cases of aplastic anemia and three cases of acute leukemia received immunosuppressive medication, chemotherapy, and hormone medicines, and one case had allo-SCT. In order to treat a fungal infection, all 5 patients received amphotericin B (1 instance was externally applied) mixed with voriconazole, posaconazole, or isavuconazole, 3 patients received amphotericin B liposomes, 2 patients received 2 medications combined, and 3 cases received 3 drugs combined. Four patients whose infections were not well managed died or actively fled the hospital as the condition worsened, and their prognosis was very bleak. Long-term survival was achieved in patients who underwent allo-SCT treatment, which involved deep and thorough debridement of the diseased location. (Table 1 for the summary of the case report)
Conclusion: Patients with significant conditions and poor prognoses, particularly those whose immune systems have been compromised, include those with hematological disorders compounded by fungal cellulitis in the craniofacial region, this calls for caution. Preventing fungus infection should be a priority. As soon as there are indications of infection, detailed tests including bacterial culture, imaging, and histology should be performed as once to identify the pathogenic bacteria. Antifungal drug therapy and extensive and complete surgical debridement should also be performed depending on the degree of tissue necrosis. For a mixed infection involving many pathogens, it is also important to determine each pathogen's therapeutic sensitivity as much as feasible in order to administer a joint anti-infection treatment.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal